Dental Health’s Connections to Mental Health
Almost one billion people globally have a diagnosed mental health disorder, including more than 3% with diagnosed depression and/or anxiety; a percentage that rises to 25-31% in adolescents(1). People with mental health disorders are three times more likely to lose their teeth than the general population(2). But what does this have to do with oral health? While some connections between mental health disorders and oral health are tangible—such as the impacts of eating disorders, excessive consumption of alcohol, and substance abuse—and some are almost universal (77% of adults agree taking action to protect oral health is closely connected to their mental health)(3), some connections are less apparent (and less studied), but equally as significant.
The Cycle of Dental Health and Mental Health
The relationship between mental health and dental health is often a cyclical one. Poor oral health can lead to embarrassment and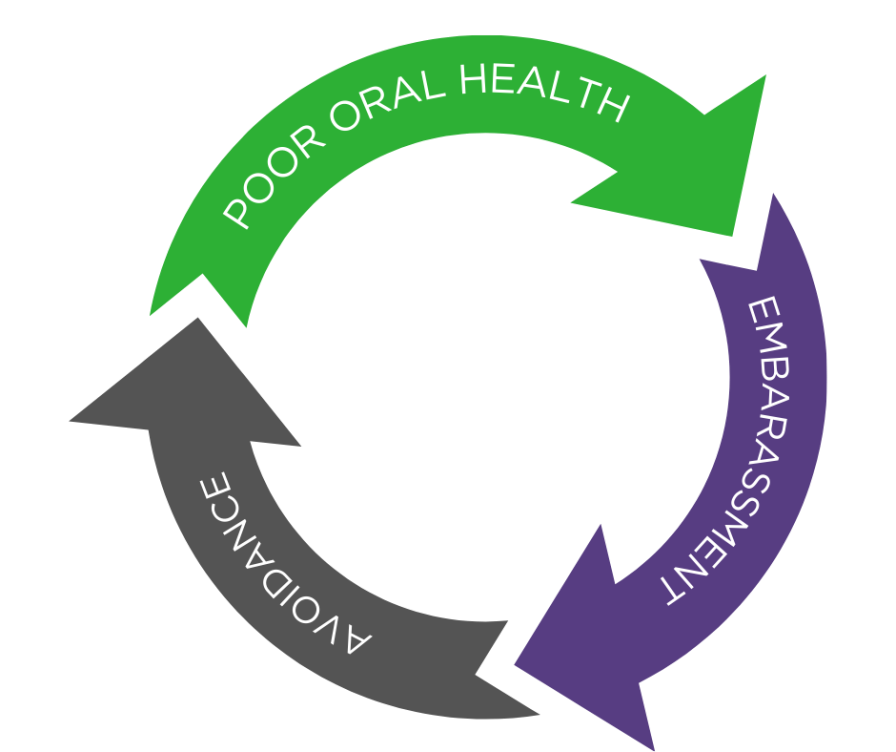
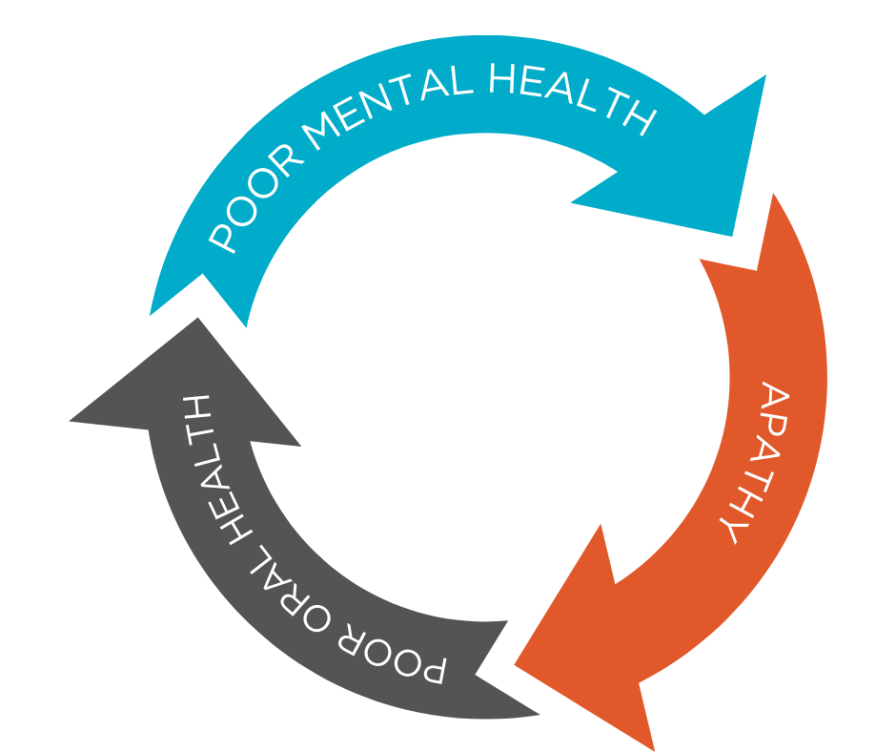 low self-esteem (often stemming from its impact on appearance), which can lead to an underutilization of dental care, which compounds poor oral health. Similarly, mental health disorders such as depression can erode healthy oral health habits and lead to apathy towards personal care. With an understanding of the complexities that inform these cycles, is it possible to break them?
low self-esteem (often stemming from its impact on appearance), which can lead to an underutilization of dental care, which compounds poor oral health. Similarly, mental health disorders such as depression can erode healthy oral health habits and lead to apathy towards personal care. With an understanding of the complexities that inform these cycles, is it possible to break them?
Understanding Dental Fear and Anxiety
There is value in understanding the different kinds of mental health disorders impacted by dental health, and vice versa, dental anxiety itself being a common one. Dental fear and anxiety (DFA) impact approximately 35% of Americans (while 12% experience an extreme dental fear)(4)and can present significant barriers to dental attendance. Among other possible sources, DFA often stems from traumatic experiences (including other people’s) and sometimes with false or inaccurate memories. Heritability and fear of bad news are also sometimes cited but research has shown that “influences from friends and family members are considered to be the most relevant when considering DFA in children” and, for adolescents, “the impact of the peer group is believed to be more important.”(4)
Delta Dental of Kansas encourages three things of patients to help reduce dental anxiety:
1. Education. Understanding the importance of preventive and at-home oral care, and their impact of the likelihood of major dental procedures has the potential to stop dental anxiety before it takes too firm a hold.
2. Conversation. We encourage patients to talk to and ask questions of their care providers, share their concerns, and advocate for their own needs.
3. Expectation. Whether it be regarding specific procedures or paying for treatment, understanding what to expect from a dental visit can reduce the fear of the unknown
It is important to note that dental phobia is a different disorder. Not interchangeable with DFA, dental phobia has been defined as “a special kind of fear, out of proportion to the demands of the situation, which will not respond to reason, is apparent beyond voluntary control and leads to avoidance of dental treatment where this is really necessary.”(4)
Dental Health’s Relationship with Specific Mental Health Disorders
Various studies have explored the biological impact of oral health on specific mental health disorders. Research suggests, for example, that tooth loss is a possible risk factor for cognitive decline and dementia; one theory being the impact of tooth loss on the ability to chew, and rehabilitating patients’ masticatory function can have positive effects on their memory and cognitive functions.(1)
Periodontitis features regularly in research and studies suggest an association between it and Alzheimer’s disease.(1) It has also been linked to depression, with significant differences in the oral microbiomes of those with depression being reported. Elevated risks for bipolar disorder and Parkinsons disease—disorders in which inflammation is a factor—have been reported in those with periodontitis.(1)
The reverse also continues to be studied—how mental health disorders affect the ability to maintain adequate oral hygiene. Factors include a decline in motor functionality and the cycle of shame and low self-esteem discussed above. Again, periodontitis is a great example of this—patients with periodontic symptoms such as bad breath and tooth loss can feel obliged to isolate themselves and avoid social interactions.
Implications of Underutilization for Dentists
Regardless of the research still required to unpick mental- and dental health’s chicken and egg-like relationship, patients with mental health disorders are more likely to have poor oral health, and less likely to visit a dentist. To counter this under-utilization, dentists should consider their appointments with these patients as an overall health check.
Dential professionals have an opportunity to impact a patient's quality of life by paying particular attention to oral signs of disease elsewhere in the body, and of course, the impact of their mental health disorder on their oral health. Dentists could also consider trauma-informed care and an integrated approach to care planning, with counsel from the patient’s primary- and other care providers. In addition, dental hygienist consults (often a patient’s first and most intimate interaction) can play a key role in identifying and mitigating DFA.
For those whose mental health disorders prohibit them from making it as far as the chair, education is powerful. Many stakeholders in a patient’s life, including their care providers, employers, peers, and insurance providers, have an opportunity to educate them about the importance of oral health and its relationship with overall health, and to help familiarize them with dentistry environments and processes. Oral Health needs to be considered by patients and care providers alike as the integral piece of a complex health puzzle it is; one without which, the world’s mental health crisis stands to worsen.
Sources
[1] Skallevold HE, Rokaya N, Wongsirichat N, Rokaya D. Importance of oral health in mental health disorders: An updated review. J Oral Biol Craniofac Res. 2023 Sep-Oct;13(5):544-552. doi: 10.1016/j.jobcr.2023.06.003. Epub 2023 Jun 19. Erratum in: J Oral Biol Craniofac Res. 2024 Jul-Aug;14(4):353-354. doi: 10.1016/j.jobcr.2024.05.011. PMID: 37396968; PMCID: PMC10314291.
[2] Choi J, Price J, Ryder S, Siskind D, Solmi M, Kisely S. Prevalence of dental disorders among people with mental illness: An umbrella review. Aust N Z J Psychiatry. 2022 Aug;56(8):949-963. doi: 10.1177/00048674211042239. Epub 2021 Aug 30. PMID: 34461748.
[3] Delta Dental Plans Association, 2024
[4] Beaton L, Freeman R, Humphris G. Why are people afraid of the dentist? Observations and explanations. Med Princ Pract. 2014;23(4):295-301. doi: 10.1159/000357223. Epub 2013 Dec 20. PMID: 24356305; PMCID: PMC5586885.
